Research Shows COVID-19 Pandemic Reduction in Claims Skews Data for 2021 Medicare Advantage Risk Scores
Reduction in service utilization leads to insufficient data to determine 2021 MA risk scores and payment
Washington, D.C. – Better Medicare Alliance (BMA), the leading research and advocacy organization supporting Medicare Advantage, unveiled new research conducted by Avalere Health. The findings show that the drop in Medicare Advantage claims data from patients who have forgone routine care due to the COVID-19 pandemic will likely lead to insufficient data to properly determine Medicare Advantage risk scores in 2021, with impact on payment.
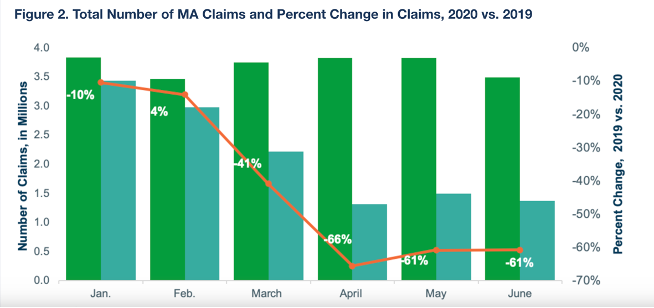
The analysis, commissioned by BMA, examined Medicare Advantage claims data through June 2020 and found that total Medicare Advantage claims dropped 66% in April 2020 from 2019 and remained 61% lower in May and June as compared to the same months a year earlier.
As Avalere’s research explains, “Lower utilization results in fewer opportunities for providers to code diagnoses.” The Centers for Medicare. & Medicaid Services (CMS) uses diagnosis data from claims to calculate MA risk scores used to adjust payments to MA plans.
Because diagnoses from 2020 claims are used as an input to determine 2021 risk scores, fewer claims in 2020 mean less data to properly inform risk scores and may result in risk scores that do not accurately reflect the true health status of beneficiaries. Avalere estimates a 6.3% – 9.6% decrease in risk scores that would lower payment to Medicare Advantage by 4.2% to 6.14% in 2021.
“The Medicare Advantage community’s response to COVID-19 has mitigated the harm of this virus on our most vulnerable seniors. As this research shows, however, beneficiaries who were not directly impacted by COVID-19 largely stayed home – postponing routine care and leading to a sharp drop in Medicare Advantage utilization,” said Allyson Y. Schwartz, President and CEO of the Better Medicare Alliance. “Medicare Advantage’s ability to properly care for its 25 million beneficiaries is built on accurate, stable payment that captures the health status of enrollees. This research demonstrates the significant impact of the COVID-19 pandemic on this process. With these figures in hand, we will continue to monitor service utilization and insist that every effort is made by CMS to allow health plans to gather the data needed in the midst of the ongoing pandemic and, as needed, make appropriate adjustments to ensure decisions are based on complete information. Beneficiaries deserve nothing less.”
Avalere’s analysis also explained how new telehealth flexibilities likely prevented a further reduction in service utilization, noting that telehealth utilization increased to 21% of all claims in April 2020 as compared to 5% the year earlier.
Read the full analysis from Avalere HERE.
###
