A look at the Medicare Advantage community’s
response to COVID-19 for seniors
With seniors among those most at risk from COVID-19-related complications and even death, the importance of protecting our nation’s Medicare beneficiaries during the ongoing pandemic is critical.
When COVID-19 struck, Medicare Advantage was ready to respond to new challenges and meet beneficiary needs. Medicare Advantage is lowering out-of-pocket expenses, offering additional benefits such as meal services and transportation, and enhancing touchpoints with providers that are not available in Traditional Medicare.
Working together, Medicare Advantage waived consumer costs, supported humanitarian relief efforts, and facilitated a swift transition to virtual care in order to keep beneficiaries healthy and safe at home.

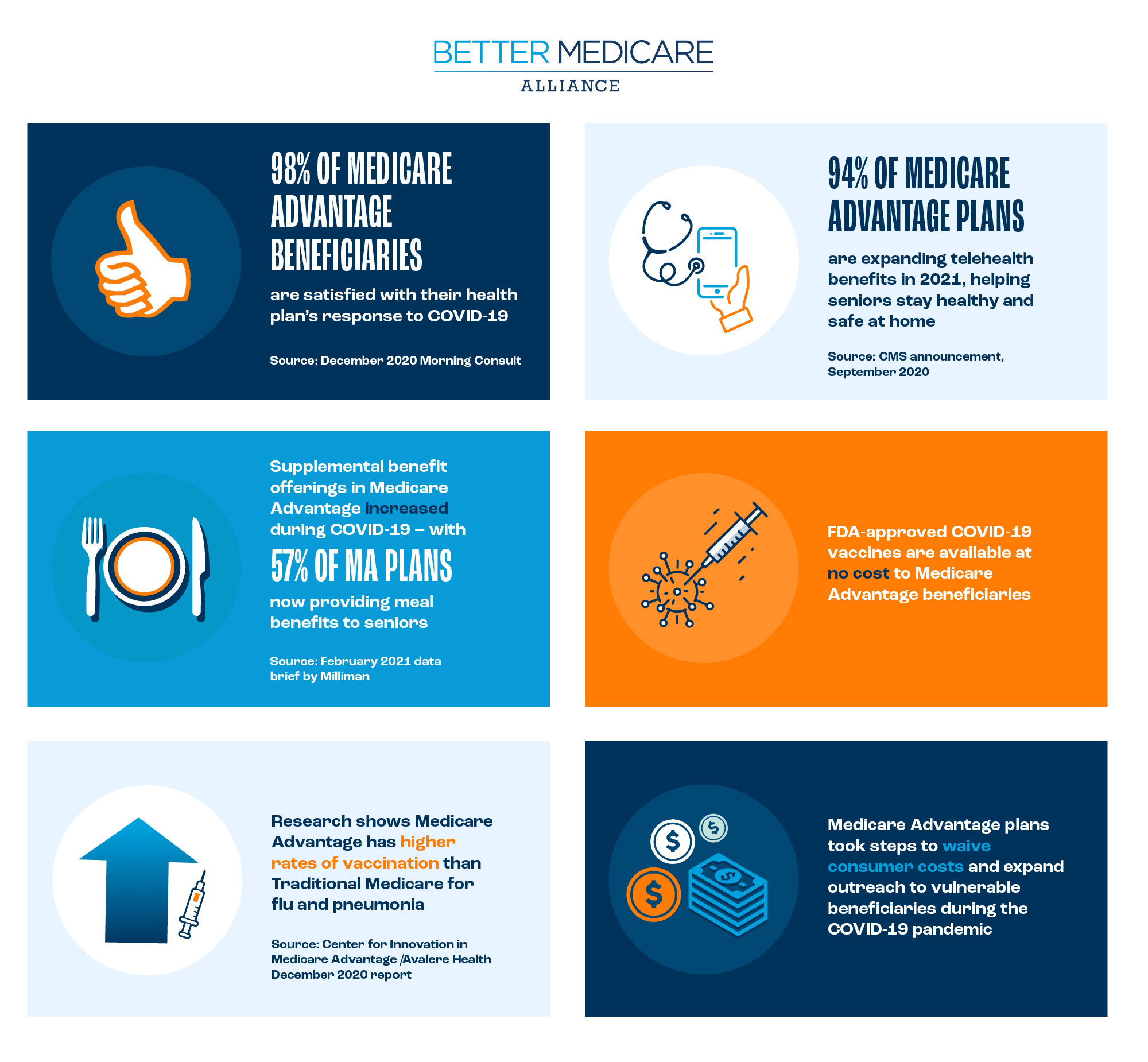
Throughout the COVID-19 pandemic, Medicare Advantage is taking unprecedented steps to help beneficiaries, including by covering the full expense of in-network COVID-19 medical treatment, while many Medicare Advantage primary care providers delivered tablets and made home visits to beneficiaries to help them complete appointments. Health plans, multi-specialty group, and primary care practices, as well as those with high-risk Medicare Advantage populations, engaged in personalized outreach to those who were socially isolated to ensure they have access to care and supportive services.
A July 2020 report from the Center for Innovation in Medicare Advantage detailed how Medicare Advantage’s payment structure and flexible benefit design ensured faster adoption of telehealth and in-home services during the pandemic. While telehealth adoption increased significantly in Traditional FFS Medicare during the pandemic as well, the report found that, “Traditional FFS Medicare policies have slowed the uptake of telehealth generally and served as a barrier to telehealth implementation and expansion.”
In 2021, Medicare Advantage continues to leverage supplemental benefits to meet beneficiary needs arising from COVID-19. More than half of all Medicare Advantage plans provide a meal benefit that can help keep seniors healthy and safe at home, while CMS reports that over 94% of Medicare Advantage plans are providing expanded telehealth benefits for 2021.
Firsthand Stories of How #MAresponds
Read a sampling of inspirational stories from our Ally organizations explaining firsthand how #MAresponds to the ongoing COVID-19 pandemic
Aetna/CVS Health
Aetna eliminated barriers to care by waiving cost-sharing for COVID-19 testing and treatment, in-network primary care office visits, and all telehealth care for Aetna Medicare Advantage members. What’s more, Aetna shipped “Caring for You” kits containing items like face masks, hand sanitizer, and thermometers to 2.7 million Aetna Medicare Advantage members– helping them stay safe and healthy during the pandemic. Additionally, CVS Health tested more than 15 million people for COVID-19 through CVS Health facilities and has already administered nearly four million vaccine doses to long-term care facility residents and staff, helping to protect one of our most vulnerable populations.
Banner Health
In response to the COVID-19 pandemic, Banner Health was quick to expand virtual care offerings and telemedicine capabilities to all of its 28 hospitals. In November 2020, Banner Health in partnership with Northwest Healthcare rolled out its own Medicare Advantage plan – becoming the only non-profit and locally based Medicare plan in Arizona.
Commonwealth Care Alliance
During the COVID-19 pandemic, Commonwealth Care Alliance launched a quality initiative program aimed at improving care for seniors and offered up to $1.05 million in funding to Federally Qualified Health Centers. They’ve also provided medical and behavioral health services to the Massachusetts COVID-19 Response Command Center and clinical partners, along with awarding the Lowell Community Health Center (LCHC) $50,000 to address gaps in care for individuals with chronic conditions.
ChenMed
Even before the COVID-19 pandemic began, ChenMed regularly checked in on patients with what they call “love calls” – and effort that has only increased during the pandemic. ChenMed has provided masks to seniors, iPads to help them with telehealth options, and even delivered toiletries and groceries. Recently, a study of 400 ChenMed patients showed how value-based care – which has proliferated across Medicare Advantage – may reduce deaths among high-risk COVID-19 patients.
Doctor on Demand
Following CMS’s expansion of telehealth flexibilities during the COVID-19 pandemic, Doctor on Demand became the first full-service telehealth provider to more than 33 million Medicare Part B beneficiaries. They also went on to waive copays for all medical services for Medicare Part B during the COVID-19 pandemic. Additionally, Doctor on Demand raised $75 million to expand its virtual primary care and behavioral health platform.
Humana
During COVID-19, Humana’s ongoing focus is simplifying access to care, reducing financial barriers, and addressing social determinants of health for its most vulnerable members and communities. Humana has offered at-home testing for COVID-19, mailed 1 million in-home preventative screening kits to members, and dedicated a concierge phone line to COVID-19 related inquiries. The Humana Foundation also invested $3 million in the national nonprofit Older Adults Technology Services (OATS) to establish and lead Aging Connected – an effort dedicated to getting at least 1 million disconnected seniors online, particularly those in marginalized communities. Humana staff have delivered more than 1.3 million meals to individuals experiencing food insecurity during the pandemic
Iora Health
Iora Health is an innovative value-based primary care provider for seniors with locations around the country. Iora co-founder Dr. Rushika Fernandopulle explained at a February 2021 BMA webinar how his organization responded to the COVID-19 pandemic, saying “Over a weekend, we transformed all of our care. We kept all of our practices open … we shifted 92% of our encounters to telehealth … we figured out lots of ways to help seniors with video who had trouble with that. The other thing we did over the first two weeks is we reached out to every one of our patients – we reached over 90% in two weeks – and said ‘we are here for you, we’re open 24/7.’” Even in 2021, Iora continues to conduct more than 50% of its patient encounters over video. For patients who lack the technology to complete appointments via telehealth, Iora has delivered sanitized, pre-configured tablets to patients’ homes. Dr. Fernandopulle praised Medicare Advantage’s value-based framework and flexible benefit design as being critical to Iora’s ability to nimbly respond to the pandemic, adding “Medicare Advantage is the fuel that lets us work.”
Meals on Wheels America
Meals on Wheels America has been delivering meals and addressing social isolation among seniors since 1969. By July of 2020, Meals on Wheels’ COVID-19 Response Fund had served 47% more seniors than pre-pandemic and saw a 77% increase in the number of meals they distributed. During a recent BMA webinar, Lucy Theilheimer, Chief Strategy and Impact Officer at Meals on Wheels spoke on the importance of Medicare Advantage to Meals on Wheels’ success, saying “The opportunity with Medicare Advantage is to be able to extend the reach and impact for a broader range of services … some of those non-health-related wraparound services are so essential to keeping people healthy and keeping them independent in their homes.”
Northwell Health
As New York State’s largest health care provider, Northwell Health knew it needed to find ways to keep seniors out of the of the hospital and safe at home during the pandemic. To address this challenge, Northwell Health launched a home-based care program for people infected with COVID-19 and expanded their telemedicine services. In their effort to reduce beneficiary costs during the COVID-19 pandemic, Northwell Health eliminated additional costs for in-network primary care, outpatient behavior health, and telehealth visits for its Medicare Advantage beneficiaries.
Oak Street Health
When COVID-19 struck, Oak Street Health knew it needed to find ways to keep seniors safe at home, while accounting for the fact that many of their beneficiaries would not be immediately comfortable with traditional audio-video telehealth visits. Instead, Oak Street met seniors where they are by providing simply telephone visits – something that would be harder to do under Traditional FFS Medicare. “We’re not driven by fee-for-service economics, we don’t care if something is billable,” explained Oak Street’s CEO Mike Pykosz to Fierce Healthcare.
The New England Journal of Medicine also detailed how Oak Street began proactively calling patients to ensure their basic needs were met during the pandemic –reporting an increase of about 60% in daily patient encounters. Oak Street Health additionally repurposed its own fleet of pickup vans into a delivery service for food and groceries. Between mid-March and July 2020 alone, Oak Street Health completed close to 9,000 food deliveries.
Papa
When the pandemic hit, Papa was already a step ahead. Papa provides companionship for seniors and help with everyday tasks, including: grocery delivery, technology lessons, transportation services, and others. Over the past year Papa has expanded its services to all 50 U.S. States and has grown 600% year-over-year. Papa also continues its work on addressing social isolation and healthcare needs for seniors and Medicare Advantage members through partnerships with telehealth companies like Flexcare and collaborations with Medicare Advantage plans like Alignment Healthcare.
SCAN Health Plan
During the COVID-19 pandemic, SCAN Health Plan conducted outbound phone calls to check in on vulnerable Medicare Advantage beneficiaries and address preventive needs. To date, an estimated 160,000 phone calls have been made to members. SCAN also created a team to help members with social support issues who might need meals, groceries, masks, access to care, or technology assistance. More than 30,000 meals have been provided through this effort. Additionally, SCAN is partnering with community-based organizations and hospitals to find available COVID-19 vaccine open appointments for their most vulnerable beneficiaries – including arranging transportation and registering them for the appointment.
Tivity Health
Tivity Health brings fitness and social connection to over 16 million Medicare Advantage members through its SilverSneakers program. When the COVID-19 pandemic began, SilverSneakers created over 200 on-demand workout videos that members can view online from the safety and comfort of home. SilverSneakers also began providing free workout videos to their community of more than 900,000 Facebook followers. In places with relatively low COVID-19 transmission rates, SilverSneakers has also continued to provide socially distanced fitness classes outdoors.
Tufts Health Plan
Tufts Health Plan is partnering with local organizations to reach communities of color that are disproportionately impacted by COVID-19 – providing educational resources and combating vaccine hesitancy among these populations. The Tufts Health Plan Foundation joined with the Harvard Pilgrim Health Care Foundation to make a joint $1 million community investment supporting COVID-19 vaccine education in communities of color.
UnitedHealth Group
UnitedHealth Group is providing over $1.5 billion in support to customers – including Medicare Advantage beneficiaries by –waiving cost-sharing; contributing to relief efforts; launching a free nationwide emotional support line; providing unlimited telehealth; and deploying 200,000 kits to seniors that include Tamiflu, the prescription antiviral treatment, a digital thermometer; and a coronavirus P.C.R. diagnostic test.
UPMC Health Plan
UPMC Health Plan continues to waive all deductibles, coinsurance, and copays for in-network, inpatient COVID-19 treatment among its. Medicare Advantage members through April 20, 2021. UPMC Health Plan also continues to waive member cost sharing for in-network telehealth visits with a health care provider—including through UPMC AnyWhereCare—until April 20.








