BMA Issues Bold Recommendations to Strengthen Protections for Seniors, Maintain Transparency in Medicare Advantage
Alliance calls on CMS to adopt a comprehensive approach to Medicare Advantage audits, including auditing every plan every year and applying future audit changes prospectively
Washington, D.C. – As the Centers for Medicare & Medicaid Services (CMS) prepares to issue Medicare Advantage rulemaking for 2024 and beyond, Better Medicare Alliance unveiled a groundbreaking set of recommendations designed to build upon the success of Medicare Advantage and improve the value of the program for seniors.
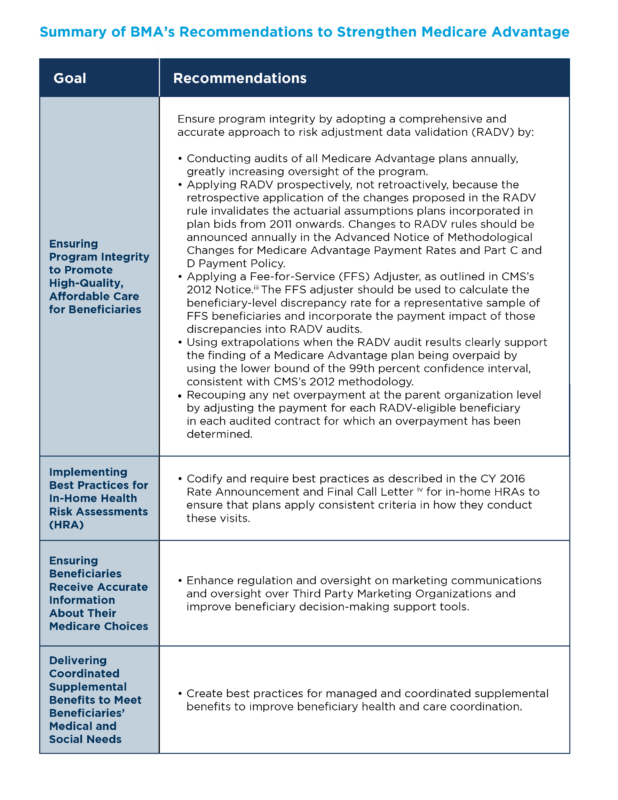
“Sustaining and Strengthening Medicare Advantage: Policy Recommendations to Maintain Accountability and Support Beneficiaries,” calls for a comprehensive approach to Medicare Advantage Risk Adjustment Data Validation (RADV) audits – including auditing every plan every year, better identifying and treating beneficiaries’ needs using in-home health risk assessments (HRAs), giving beneficiaries the information and support they need to choose the right plan based on their unique needs, and realizing the full potential of supplemental benefits to improve senior health.
“Policymakers are weighing important decisions about the future of more than 29 million Americans’ Medicare Advantage coverage. With these recommendations, we are offering new solutions to inform an even more transparent, accountable Medicare Advantage that continues to provide exceptional value for beneficiaries and taxpayers alike,” said Mary Beth Donahue, President and CEO of the Better Medicare Alliance. “Medicare Advantage delivers a 94% satisfaction rate, nearly $2,000 in average annual consumer savings, and lower per-beneficiary government spending – and still we know there are opportunities to further strengthen this vital part of the Medicare program. These recommendations offer a necessary path forward.”
Recommendations include:
- Audit every Medicare Advantage plan annually: CMS should conduct RADV audits of all Medicare Advantage plans annually, just as it already does for health plans offered on the Affordable Care Act (ACA) marketplace, to increase program oversight and ensure that arbitrary decisions about which contracts are audited do not disproportionately impact some organizations more than others. Ensuring parity with ACA auditing practices would support stability for beneficiaries and increase confidence in CMS’s Medicare sustainability efforts.
- Changes should be prospective, not retroactive: Changes to audit methodologies should be applied prospectively, not retroactively. A retrospective application of audit changes currently under consideration at CMS would invalidate actuarial assumptions made by health plans over more than a decade and threaten the care that seniors rely on today.
- Implement best practices for in-home HRAs: As an integral part of Medicare Advantage’s unique care coordination model, in-home HRAs are primarily used for preventative care and to assess the overall health of beneficiaries, document diagnoses, and identify gaps in care and unmet needs based on the information collected. BMA believes that in order to ensure all in-home HRAs are high-quality and delivering value to the beneficiary, CMS should codify a robust set of best practices for these evaluations. Doing so would ensure that plans apply consistent criteria in how they conduct in-home HRAs, prevent the use of sub-standard in-home HRAs that are not providing clinical value, and promote access to holistic primary care.
- Ensure beneficiaries receive accurate information about their Medicare choices: Accurate marketing of Medicare Advantage plans is essential for beneficiary education, choice, and trust in the Medicare program.BMA calls on CMS to enhance guidance to improve Medicare Advantage plans’ oversight of third-party marketing organizations (TPMOs). BMA further supports continued improvements to beneficiary decision-making support tools.
- Deliver coordinated supplemental benefits to meet beneficiaries’ medical and social needs: As Medicare Advantage plans continue to incorporate new supplemental benefit flexibilities into their strategies for providing holistic care for beneficiaries, BMA recommends that plans and policymakers work together to ensure that Medicare Advantage provides coordinated supplemental benefits rather than cash benefits to ensure beneficiaries are accessing services that will meet their health needs. BMA further supports efforts to ensure health plans tailor member benefits for best health (e.g., promote and provide access to nutritional foods) so that beneficiaries receive services that align with their care plans and provide support and guidance to beneficiaries on accessing and using member benefits to increase uptake.
Health policy leaders applauded the recommendations, including:
“Policymakers need not accept a false choice between protecting seniors’ Medicare Advantage coverage and identifying opportunities to further strengthen the program’s high bar of transparency and accountability. Better Medicare Alliance’s recommendations offer a path for our leaders to accomplish both goals,” said Kenneth Thorpe, PhD, Chair of the Department of Health Policy and Management in the Rollins School of Public Health at Emory University and Chair of the Better Medicare Alliance Board of Directors. “Seniors will appreciate the calls for added oversight of third-party marketers and better tools to understand their supplemental benefits, while lawmakers will appreciate the roadmap for a rigorous and fair-minded audit process.”
“53% of Medicare-eligible Latinos today choose enrollment in Medicare Advantage. With that strong vote of support from our community also comes a unique responsibility for Medicare Advantage health plans and providers. In these recommendations, Better Medicare Alliance is bringing diverse stakeholders around the table to drive meaningful solutions that support seniors and ensure continued accountability of Medicare dollars,” said Elena Rios, MD, MSPH, MACP, President and CEO, National Hispanic Medical Association and Member of the Better Medicare Alliance Board of Directors.
“Our roughly 360 physician groups across the country know how important Medicare Advantage is to many of the 90 million-plus patients that our groups serve,” said Susan Dentzer, President and CEO, America’s Physician Groups. “In this issue brief, Better Medicare Alliance has offered forward-thinking proposals for ensuring the integrity of Medicare Advantage even as it serves a growing share of the Medicare-eligible population. Our organization’s motto is ‘Taking Responsibility for America’s Health,’ and by the same token, it’s imperative that Medicare Advantage be responsible for both enrollees’ health and the appropriate use of taxpayer dollars. We look forward to working with BMA and the nation’s policymakers to advancing and finetuning these proposals so that Medicare Advantage is even more responsible and accountable for the costs and high quality of enrollees’ care.”
“Better Medicare Alliance’s recommendations will better position the program to continue delivering transparent affordable coverage seniors and the disabled deserve,” said Joel White, President of the Council for Affordable Health Coverage.
To read the full report, click here.
###
