
Direct Contracting and Medicare Advantage: Understanding the Differences
By Jonathan Frank
When individuals become eligible for Medicare, they face an important decision: whether to enroll in fee-for-service (FFS) Medicare – sometimes called Traditional Medicare – or Medicare Advantage.
As our 2022 State of Medicare Advantage report shows, more than 28 million Americans now choose enrollment in Medicare Advantage; a figure that has doubled over the last decade as beneficiaries continue to see significant cost savings, better health outcomes, and high overall satisfaction.
But for those who remain in FFS Medicare, regulatory changes over the last three years have meant some beneficiaries could still receive care under a delivery model that bears certain similarities to Medicare Advantage.
Background on Direct Contracting
In 2019, the Centers for Medicare & Medicaid Services launched direct contracting (formally known as the Global and Professional Direct Contracting Model), a voluntary payment model that allowed health systems, primary care practices, clinics, health plans and other health care organizations to enter into risk-sharing agreements with CMS for FFS Medicare beneficiaries’ care.
As Healthcare Dive explains, “The original direct contracting model was launched to coordinate primary and specialty care, while giving access to enhanced benefits in Medicare, like telehealth visits and help with co-pays. The model, in which physicians can accept either full or partial capitation as payment, offers higher levels of risk and reward … while providing additional flexibilities.”
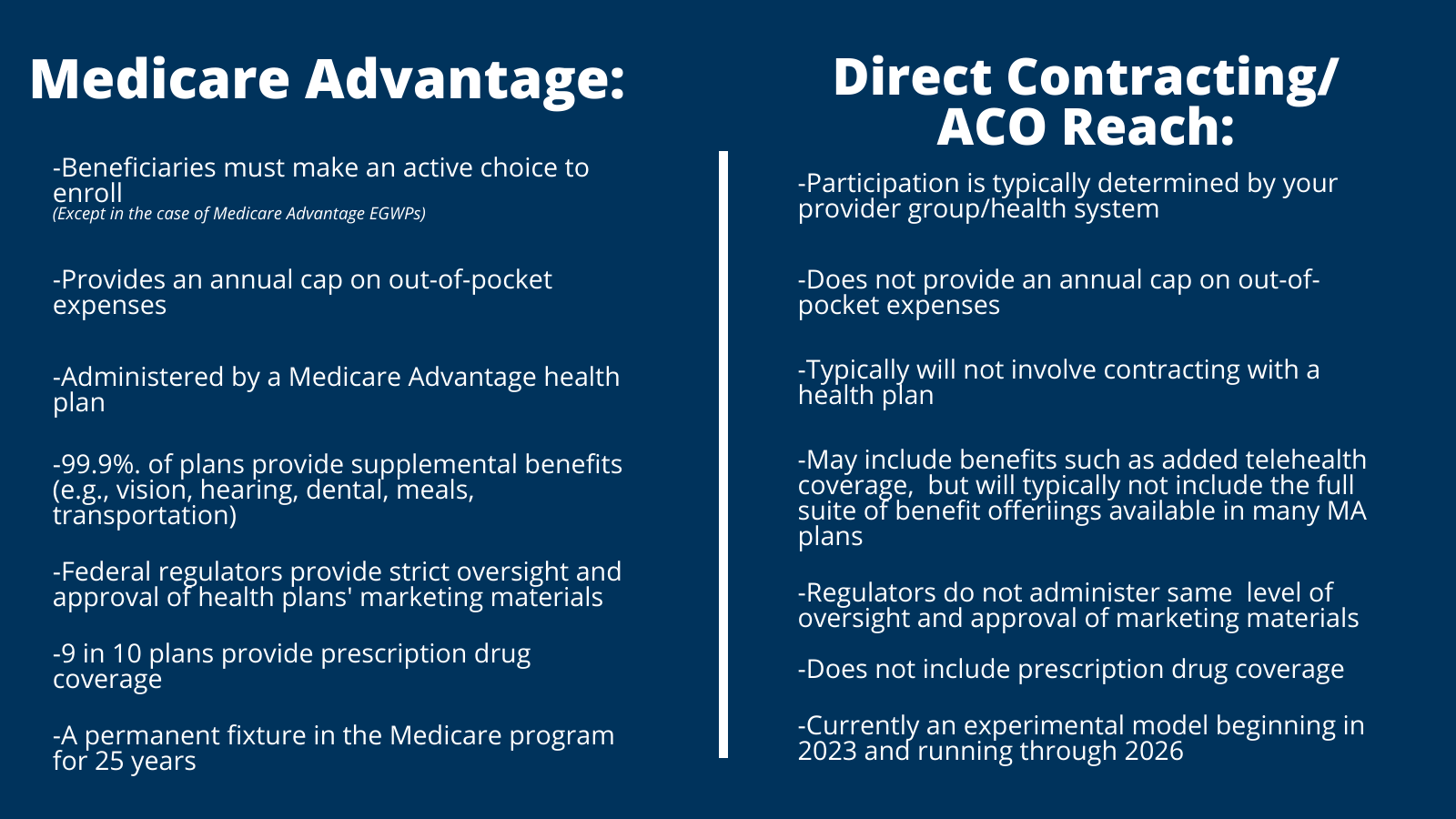
In other words, direct contracting applied certain incentives and flexibilities from Medicare Advantage, but without some of its protections and without the presence of a Medicare Advantage plan. Other important distinctions applied too. For example, beneficiaries who receive care from a provider using direct contracting would not typically have the safeguard of an annual cap on out-of-pocket expenses like Medicare Advantage beneficiaries do.
Likewise, while direct contracting may offer additional telehealth benefits than one might typically receive in FFS Medicare, there is not the same access to a wide array of supplemental benefits – from dental, vision, and hearing coverage, to meal delivery and even transportation between medical appointments – that many Medicare Advantage beneficiaries receive. Neither does direct contracting include prescription drug coverage. 89% of Medicare Advantage plans provide an integrated prescription drug benefit.
Further, whereas enrollment in Medicare Advantage is an active choice that a beneficiary must make for themselves, beneficiaries could be receiving services from a provider using direct contracting without necessarily knowing (notification would typically come after the fact through a letter mailed to the beneficiary).
Transitioning to ACO REACH
Earlier this year, CMS effectively ended this earlier iteration of direct contracting and replaced it with the Accountable Care Organization (ACO) Realizing Equity, Access, and Community Health (REACH) Model, set to launch on January 1, 2023 and continue through 2026.
While ACO Reach includes stricter oversight measures and a renewed focus on health equity, the core functions of direct contracting are preserved. CMS says the new payment model will seek to “improve the quality of care for people with Medicare through better care coordination, reaching and connecting health care providers and beneficiaries, including those beneficiaries who are underserved.”
Not Medicare Advantage
Whether in its original form or under the new parameters of ACO REACH, direct contracting is not Medicare Advantage. Regrettably, some media coverage and opinion articles have conflated and confused these two distinct programs in recent months.
For example, a recent column argues that “Under the Direct Contracting Entities (DCE) program … more seniors are being automatically enrolled into [Medicare] Advantage programs, often without their knowledge or permission.”
This is false. Beneficiaries who receive care from a provider participating in direct contracting are still enrolled in FFS Medicare. As CMS explains, “Beneficiaries [in ACO REACH] with Traditional Medicare retain all of their rights, coverage, and benefits.” It remains illegal to enroll a beneficiary in Medicare Advantage without their knowledge or consent. This infographic helps to further explain some of the major differences between these two programs:
Better Medicare Alliance’s perspective
As an organization with a singular focus on protecting and strengthening Medicare Advantage for our nation’s seniors, Better Medicare Alliance does not engage in advocacy related to direct contracting/ACO REACH, which is an altogether different program.
We continue working to increase understanding of Medicare Advantage and the framework that enables its 94% satisfaction rate, nearly $2,000 in annual cost savings to consumers, better health outcomes, and lower per-beneficiary government spending.
Better Medicare Alliance supports policies that provide every beneficiary an opportunity to be an active, informed chooser in their health coverage.
Jonathan Frank is the Vice President of Communications at Better Medicare Alliance.
