New Analysis Highlights Innovative Approaches to Behavioral Health Coverage in Medicare Advantage
As more than one-third of Medicare Advantage beneficiaries report a behavioral health condition, research shows models of success and policy opportunities for greater access to care
Washington, D.C. – Better Medicare Alliance, the nation’s leading research and advocacy organization supporting Medicare Advantage, today unveiled a new mixed-methods analysis conducted by ATI Advisory, which shows how Medicare Advantage provides beneficiaries with access to behavioral health services that can drive better health outcomes, while identifying policy opportunities to further improve access to behavioral health care for seniors and people with disabilities.
The brief depicts how Medicare Advantage continues to serve a more medically complex beneficiary population than fee-for-service (FFS) Medicare when it comes to behavioral health needs. Medicare Current Beneficiary Survey (MCBS) data shows that Medicare Advantage beneficiaries have slightly higher rates of any mental health condition, including higher rates of depression, serious mental illness, and cognitive impairment than their FFS Medicare counterparts.
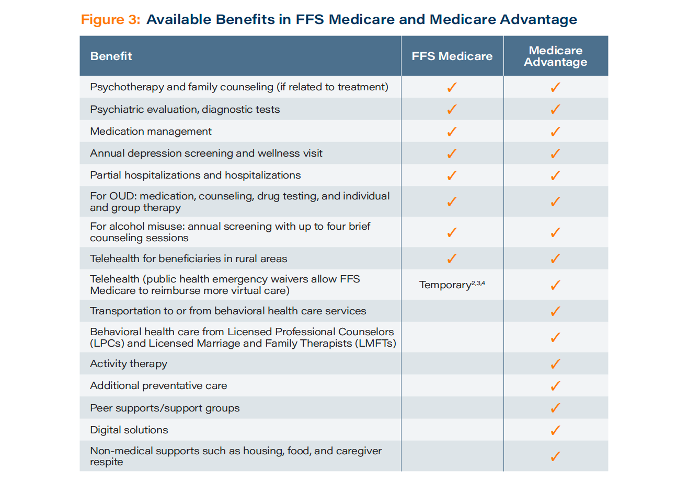
ATI Advisory’s research also demonstrates that Medicare Advantage has unique tools at its disposal to meet behavioral health needs, writing, “Because the Medicare Advantage program is able to (and does) offer services beyond what is covered in FFS Medicare, it is well-positioned to fill gaps in services by, for example, providing telehealth or transportation to appointments.”
Medicare Advantage offers a wide array of behavioral health-related benefits that may not be available in FFS Medicare, the analysis finds. For example, 83% of Medicare Advantage plans provide individual mental health telehealth coverage, while more than half (55%) provide individual substance abuse telehealth services.
MCBS data additionally shows that Medicare Advantage beneficiaries with any mental health condition and those with serious mental illness report higher rates of having a usual source of care than beneficiaries with the same conditions in FFS Medicare, as well as higher rates of having one provider who knew all their medications.
Finally, ATI Advisory’s research offers three case studies demonstrating how Medicare Advantage is approaching behavioral health services for the communities it serves, while also identifying “opportunities to address insufficient provider supply, improve coordination of services, and encourage a culture of preventive services” across the entire Medicare population.
“The COVID-19 pandemic has opened up long overdue conversations on behavioral health care needs. This research shows how Medicare Advantage is rising to the task and innovating to serve the more than one-third of beneficiaries who report a behavioral health condition. As a result, Medicare Advantage beneficiaries with a behavioral health condition are more likely to have a usual source of care and a single provider who knows all their medications than similar beneficiaries in fee-for-service Medicare,” said Mary Beth Donahue, President and CEO of the Better Medicare Alliance. “With continued bipartisan policy support in Washington, the Medicare Advantage community can do even more. As lawmakers consider future behavioral health reforms, this data brief offers helpful insights to inform their efforts.”
“Our analysis shows that Medicare beneficiaries with mental health conditions are significantly more likely than beneficiaries without mental health conditions to be low income, dually eligible for Medicaid, and experience social needs like food insecurity. These differences are exacerbated among Black and Latino beneficiaries with mental health conditions, who are almost twice as likely to be low-income compared to white Medicare beneficiaries with mental health needs,” noted Laura Benzing, lead data analyst for the study at ATI Advisory. “These findings indicate the need for diverse and innovative approaches to addressing mental health, given the strong overlap between mental health and other structural and social determinants of health.”
“Behavioral health care services are an essential component of whole-person, wraparound care for which Medicare Advantage is known. With a beneficiary population that is more likely to report a behavioral health condition than fee-for-service Medicare, Medicare Advantage has a unique responsibility in this area. Interestingly, ATI Advisory’s research shows that Medicare Advantage plans are indeed stepping up with solutions that identify unmet behavioral health needs and connect beneficiaries to the right care and support,” said Pamela Greenberg, MPP, President and CEO of the Association for Behavioral Health and Wellness (ABHW).
“More than 261,000 Nevadans choose and rely on Medicare Advantage to meet their health needs, including many who face a behavioral health diagnosis,” said Diego Trujillo, CEO of Las Vegas HEALS. “This research offers profiles in innovation, with case studies showing how health plans are using digital apps, team-based care management, and unique community-based approaches to identify unmet behavioral health concerns and protect seniors’ wellbeing above and beyond what the FFS model makes possible. As a nonprofit community of over 28,000 health care professionals in the Silver State, we call upon policymakers to strengthen and build upon these innovations in Medicare Advantage while continuing to improve behavioral health access across the Medicare population.”
“findhelp works every day to connect all people in need to behavioral health services and a host of other programs that serve them. This research shows what many have already witnessed firsthand: our partners in Medicare Advantage increasingly offer benefits and care coordination specifically tailored to address behavioral health needs,” said Erine Gray, Founder and CEO of findhelp. “The case studies included in this report merit careful consideration as lawmakers work to advance solutions that provide a brighter future for the millions of Americans facing a behavioral health condition.”
Read the full data brief from ATI Advisory here.
###
